The introduction of final wellness regulations will cause many employers to step back and reevaluate their wellness initiatives. The modified definitions for “participatory” and “health-contingent” along with the significant change to the “reasonable alternative standard” for health-contingent programs, will influence how wellness initiatives are designed and implemented. These regulatory changes, along with the IRS proposed regulations released back in May addressing affordability and minimum value determinations, will impact employer strategy in many cases also. Well designed wellness programs can produce a good ROI and boost employee morale at the same time; this does not change with the advent of these new final regulations. Employer will just need to take a little extra time to understand the new rules of the game so that whatever type of program they offer, participatory or health-contingent, the proper modifications can be made.
Revisiting the HIPAA Wellness Regulations
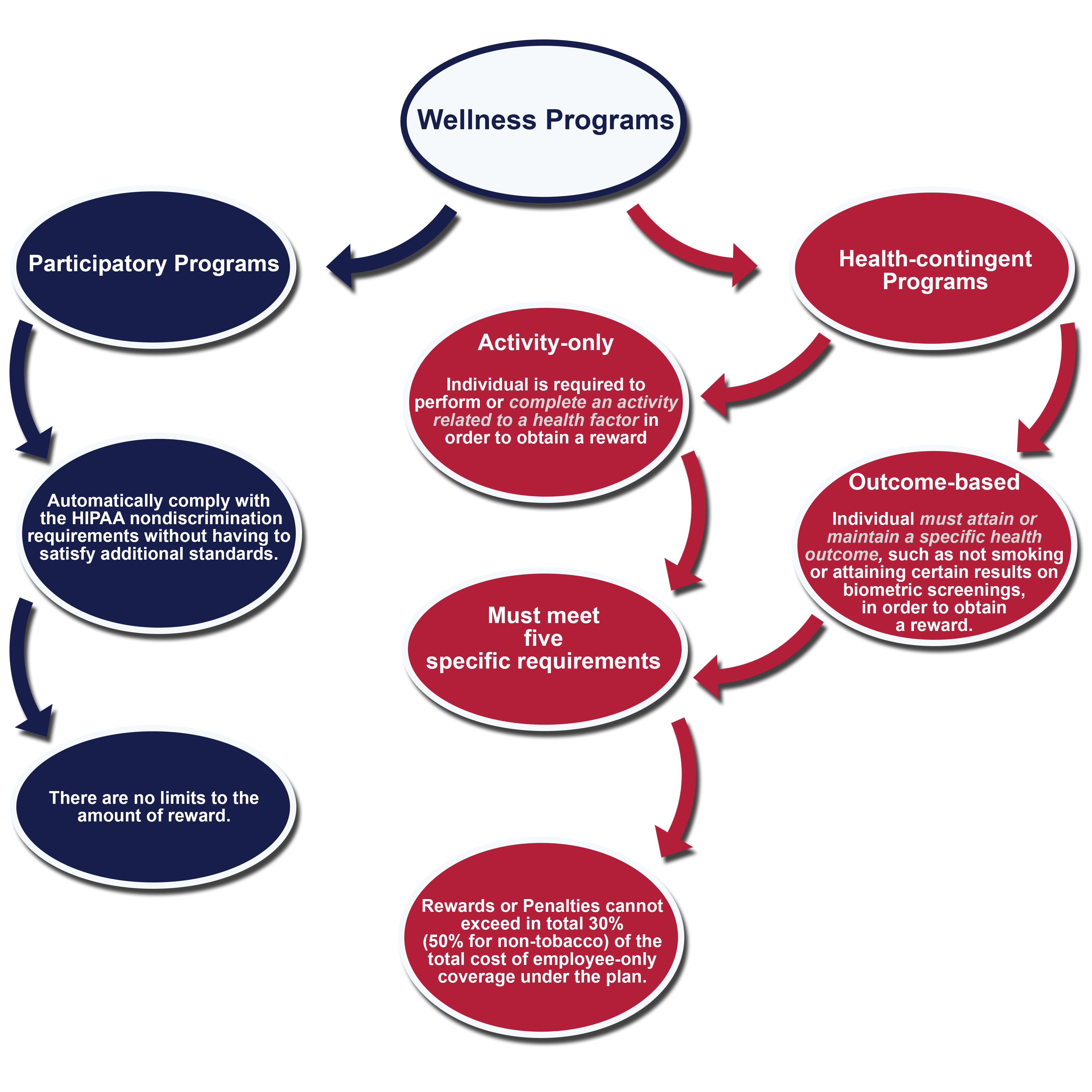
HIPAA nondiscrimination and wellness provisions that have been in place since 2006 generally prohibit group health plans and group health insurance issuers from discriminating against individual participants and beneficiaries for plan eligibility, benefits and premiums based on an individual’s health status. An exception to the existing rules has allowed premium discounts, rebates or other modifications to cost sharing in return for adherence to certain programs that promote health and disease prevention. The regulations have divided the wellness and prevention programs (we call them wellness programs) into two different categories: participatory wellness programs and health-contingent wellness programs.
Participatory Wellness Programs
These programs comply with the HIPAA nondiscrimination requirements without having to satisfy additional standards or requirements if participation in the program is made available to all similarly situated individuals regardless of health status. Any distinctions among the participants must be based on a bona fide employment classification consistent with the employer’s business practice.
Examples of participatory programs:
1. Reimbursement for participation in a fitness center.
2. A diagnostic testing program that provides a reward for participation in the program regardless of outcomes.
3. Reward provided to health plan participants who attend no-cost health seminars.
If factors other than health status limit a participants ability to take part in the program, this does not mean that the plan has violated the general rule prohibiting discrimination because the program was not discriminatory under the HIPAA nondiscrimination rules to begin with.
Example:
If all similarly situated individuals at an employer were provided the opportunity to attend an educational seminar, but a particular individual was unable to attend because the seminar was scheduled at a time the individual was unavailable to attend, this does not mean the program discriminated against that individual based on a health factor.
Health Contingent Wellness Programs
Under the same 2006 HIPAA regulations, plans and insurers that provide health-contingent wellness programs are permitted to vary benefits, premiums and/or contributions based on whether an individual has met the standards for the wellness program. Health-contingent wellness programs that tie incentives to whether a participant has met a particular health standard (i.e., BMI score) must meet five specific requirements.
Examples of health-contingent wellness programs:
1. A program that imposes a premium surcharge based on tobacco use.
2. A program that uses biometric screening or a health risk assessment to identify employees with specified conditions or risk factors and then provides a reward to those identified in the “healthy” range while requiring employees who are identified as outside the normal or healthy range to take additional steps to obtain the same reward. These additional steps might include a meeting with a health coach, a requirement to take a health or fitness course, a requirement to adhere to a health improvement action plan, etc.
Five Specific Requirements for Health-contingent Wellness Programs
1. Frequency for Qualification of a Reward – The program must give eligible individuals an opportunity to qualify for the reward at least once per year.
2. Size of Reward for Health-Contingent Programs – The reward for a program that has multiple components to the plan must not exceed 30% of the total cost of the employee-only coverage under the plan or 50% if the program is designed to prevent or reduce tobacco use. The final regulations do not include any detailed rules for apportioning the reward among family members participating in the program, but instead, have provided flexibility to determine the percentage of the reward applied to each participating family member as long as the method used to apportion the reward is reasonable.
3. Reasonable Design – The program must be reasonably designed to promote health or prevent disease. The program’s requirement for obtaining a reward is based on the results of a test, screening or measurement that is related to a health factor, the plan is not reasonably designed UNLESS it makes available to all individuals who do not meet the standard a reasonable means of qualifying for the same full reward.
The determination of whether a health-contingent wellness program is reasonably designed is based on all the relevant facts and circumstances and while the programs are not required to be accredited, employers can rely on practices illustrated in the CDC’s Guide to Community Preventive Services . Use of this resource will increase the likelihood the wellness program will be successful and it is encouraged as a best practice.
4. Uniform Availability & Reasonable Alternative Standards – The reward must be available to all similarly situated individuals. A reasonable alternative or waiver must be made available to any individual who has identified that due to a medical condition it is unreasonably difficult to satisfy the standard. This includes individuals for whom it is medically inadvisable to attempt to satisfy the standard.
5. Notice of Availability of Reasonable Alternative Standard – The plan must disclose in all plan materials describing the terms of the program and availability of other means to qualify for the reward or the possibility of waiver of the standard. The disclosure, which applies to both activity-only and outcome-based plans, must include contact information for obtaining the alternative standard and a statement that recommendations of an individual’s personal physician will be accommodated. If plan materials merely mention that a wellness program is available, without describing its terms, the disclosure it not required.
June 2013 Final Regulations
Final regulations released on June 3, 2013, have been designed to provide comprehensive guidance with respect to the general requirements for wellness programs. This new release identifies that all health plans, including grandfathered group health plans, are subject to the HIPAA non-discrimination requirements. Because there has been some confusion, these final regulations have been drafted to identify the criteria a health promotion or disease prevention program must satisfy in order for a wellness program to qualify for an exception to the nondiscrimination rules. These rules set forth specific criteria for an affirmative defense that can be used by plan sponsors in response to a claim that the plan has discriminated under HIPAA.
The final regulations also provide information to help plan sponsors make sure that a wellness program is reasonably designed to promote health and/or prevent disease, is not overly burdensome and is not a subterfuge for discriminating based on a health factor. The term “reward” includes both positive incentives and disincentives (or penalties).
Activity-only and Outcome-based Wellness Programs
As anticipated, the new rules split health-contingent wellness programs into sub-categories – activity-only and outcome-based plans. Now there is a clear distinction between programs requiring individuals to participate in certain activities to improve their health score versus one that bases a reward off of whether an individual is satisfying a particular health standard (i.e., member must achieve a specific BMI score). The Departments intend to provide further sub-regulatory guidance that will provide additional clarity and they may propose modifications to the final rule.
Example of an activity-only program:
A walking program that bases a reward on whether individuals with high blood pressure participate in a walking program.
Example of an outcome-based program:
A program that bases a reward on whether an individual with a high BMI score reduces their BMI to a desired range.
Reasonable Alternative Standard for Activity-only and Outcome-based Programs
First, in order to satisfy the requirement, the full reward must be available to individuals who qualify for the reasonable alternative standard. This is required even if the individuals need extra time to request, establish and satisfy the reasonable alternative standard. Plans have flexibility to determine how to provide the portion of the reward corresponding to the period before an alternative was satisfied as long as the method is reasonable and the individual receives the full amount of the reward. This may even include a retroactive payment of the reward within a reasonable amount of time after the end of the wellness plan year. Employers are not permitted to provide pro rata payments over the following year (i.e., the year after the year in which the reward was to be provided).
The final regulations do not require that employers establish a particular reasonable alternative before an individual requests one as long as the alternative standard is provided upon the individual’s request. There is also flexibility to provide the same reasonable alternative for an entire class of individuals or on an individual basis.
The final regulations indicate that all facts and circumstances will be taken into account when determining whether a plan sponsor has provided a reasonable alternative standard. The following factors are illustrated in the final regulations:
- If the alternative is completion of an educational program, the plan sponsor must make the educational program available or assist the employee in finding such a program. Additionally, the plan sponsor may not require the individual to pay for the cost of the program.
- The time commitment required must be reasonable.
- If the alternative standard is a diet program, the plan sponsor is not required to pay for the cost of food, but is required to pay for any membership fees or participation fee.
- If an individual’s personal physician states that a plan standard is not medically appropriate for the individual, the plan must provide a reasonable alternative standard that accommodates the recommendations of the individual’s personal physician with regard to medical appropriateness.
The final rules indicate that an individual’s personal physician can make recommendations regarding medical appropriateness that must be accommodated with respect to any plan standard.
Tobacco Cessation
For plans that contain an initial outcome-based standard that an individual not use tobacco, a reasonable alternative standard in Year 1 may be to try an educational seminar. Any individual who attends the seminar is entitled to the full reward, regardless of whether the individual quits smoking or chewing tobacco.
For Year 2, the plan may require completion of a different reasonable alternative standard, like complying with a new recommendation from the individual’s own physician or use of nicotine replacement therapy. Once again, completion of these standards qualifies the individual for the full reward. Plan sponsors can charge employees 50% more in health plan contributions if the initial standard or reasonable alternative standard has not been met.
Plan Must Continue to Offer a Reasonable Alternative Standard
Plan sponsors cannot cease to provide an alternative standard just because each year the individual continues to request an alternative and they must continue to offer a reasonable alternative standard year after year, whether it is the same or different.
Physician Statement
Activity-only Programs – Can Require a Statement
It is permissible for plan sponsors to request a statement from an individual’s physician, if reasonable under the circumstances, that a health factor makes it unreasonably difficult to satisfy an applicable standard in an activity-only wellness program.
Outcome Based Wellness Programs – Cannot Require a Statement
The reorganized final regulations clarify that outcome-based wellness programs cannot require verification by the individual’s physician that a health factor makes it unreasonably difficult for the individual to satisfy, or medically inadvisable for the individual to attempt to satisfy, the applicable standard as a condition of providing a reasonable alternative standard. An individual must be given the opportunity to comply with the recommendations of the individual’s personal physician as a second reasonable alternative standard, but only if the physician joins in the request.
See Exhibit A below:
Activity-only Program Offered as Reasonable Alternative Standard For Outcome Based Plan
If a plan provides an alternative standard that involves an activity that is related to a health factor, then the rules for activity-only wellness programs apply to that particular component of the program. In this circumstance, plans may seek verification from a physician if the participant claims it is unreasonably difficult due to a medical condition to perform or complete the activity.
IRS Guidance – Wellness Incentives, Affordability & Minimum Value
On May 3, 2013 the IRS published proposed regulations that include guidance on the relationship of non-discriminatory wellness program incentives (or penalties) to the “affordability” and “minimum value” standards.
Minimum Value
Employers that design wellness programs that include rewards or penalties in the form of reduced or increased benefits instead of premium incentives or penalties will need to be certain the benefit reductions do not decrease coverage below “minimum value” benefits unless the benefit reduction is due to the employee not meeting the non-tobacco standard.
Affordability
Transition Relief
Wellness programs for plan years that begin before January 1, 2015 (2014 calendar year plans) may qualify for transition relief. Affordability and minimum value can be determined assuming that each employee satisfies the wellness programs incentives. This transition relief only applies to the incentives that were in effect as of May 3, 2013 and it only applies to categories of employees eligible for the program as of May 3, 2013, regardless of when the employee was hired.
Resources:
http://www.gpo.gov/fdsys/pkg/FR-2013-05-03/pdf/2013-10463.pdf
Please note that the information contained in this document is designed to provide authoritative and accurate information, in regard to the subject matter covered. However, it is not provided as legal or tax advice and no representation is made as to the sufficiency for your specific company’s needs. This document should be reviewed by your legal counsel or tax consultant before use.
Additionally, the messages and content within the Pittsburgh Health Care Reform group do not reflect the advisory services of Henderson Brothers, Inc.

To download the PDF version of this EXPERT UPDATE, please click on the link below:

